Use SIGECAPS to Manage Depression – Intro
This article is for informational purposes only and is based on personal experience. It is not intended as a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of a qualified healthcare provider with any questions regarding mental health or medical conditions.
SIGECAPS is traditionally used by health professionals as a screening tool to diagnose clinical depression.
But can the SIGECAPS mnemonic also help manage depression?
My experience is that it can.
The classic SIGECAPS depression checklist became a powerful roadmap to transform my life.
Over a decade ago, I used SIGECAPS to guide a simple habit-based plan focused on clean eating, strength training, and lifestyle changes.
The result: I lost 75 pounds in six months and climbed out of clinical depression.
In short, it changed my life.
And, if it helped me, it might help you too.
Having faced major depression head-on, I found that a roadmap like SIGECAPS can make a world of difference.
Depression is a widespread challenge, affecting millions of adults in the United States alone.
According to the National Institute of Mental Health (NIMH), over 21 million adults experience major depressive episodes each year.¹
These statistics underscore the importance of recognizing and addressing depressive disorders early, as mental illness is a significant factor in approximately 60 percent of adult suicides.
That’s where SIGECAPS comes into play.
In this article, I share how the SIGECAPS checklist can be adapted into a practical plan that uses strength training, nutrition, and daily habits to support mental and physical health.
Table of Contents
- My Experience with SIGECAPS – Introduction
- What Is the SIGECAPS Mnemonic?
- Decoding SIGECAPS: Recognizing Depressive Symptoms
- Using SIGECAPS to Manage Depression
- The SIGECAPS Checklist – Practical Habits
- SIGECAPS to Manage Depression and Anxiety – Wrapping Up
- What’s Next: Exploring More Paths to Strength and Wellness
What Is the SIGECAPS Mnemonic?
I first heard about SIGECAPS when mental health professionals used it during my diagnosis.
Later, I found it helpful as a personal roadmap to improve my mood and physical fitness.
Note: You might see this tool spelled “SIGECAPS” or “SIG-E-CAPS”—both refer to the same framework.
For simplicity, I’ll use “SIGECAPS” throughout this article.
Originally intended for clinicians, I discovered that using SIGECAPS as a framework for introspection dramatically improved my sense of well-being and confidence.
In this article, I’ll share how SIGECAPS has been a pivotal part of my journey and how you can use it as a powerful tool for personal wellness and growth.
What Does SIGECAPS Stand For?
As outlined in the DSM-5 (Diagnostic and Statistical Manual of Mental Disorders, 5th Edition), each letter of “SIGECAPS” represents a specific aspect of depression, helping clinicians assess the severity of the condition.²
The term “SIGECAPS” is derived from clinical abbreviations: “SIG,” a Latin abbreviation for ‘let it be marked,’ and “E” for energy, with “CAPS” referring to capsules.
While its origins can be fascinating, this post focuses on using this tool today to improve your mental health.
Here’s a brief breakdown of the SIGECAPS mnemonic:
- Sleep changes: Variations in sleep patterns, such as insomnia or excessive sleeping.
- Interest decline: A loss of interest or pleasure in activities once enjoyed.
- Guilt or feelings of uselessness: Excessive feelings of guilt or worthlessness.
- Energy levels: Persistent fatigue or a significant decrease in energy.
- Concentration difficulties: Problems with focus and decision-making.
- Appetite/weight fluctuations: Changes in appetite or weight, either loss or gain.
- Psychomotor retardation or agitation: Slowness in physical movements or restlessness.
- Suicidal ideation: Thoughts of self-harm or suicide.
These criteria help assess depressive symptoms, but I used them personally to track my own mental and physical health.
While not everyone will experience all these symptoms, understanding them can help you recognize patterns and seek appropriate support.
Decoding SIGECAPS: Recognizing Depressive Symptoms
Now, let’s explore how to use SIGECAPS for self-reflection and daily improvement.
Detailed Breakdown of SIGECAPS
This section provides a more detailed breakdown of SIGECAPS and actionable insights into identifying signs of depression.
“S” is for Improve Your Sleep:
Are you experiencing sleep difficulties? Are you sleeping more during the day or less at night?
Changes in sleep patterns—whether insomnia or excessive daytime sleep—are classic symptoms of major depressive disorder.
These disturbances can significantly impact your mental health and overall well-being.
“I” for Loss of Interest:
Have you lost interest in activities you once enjoyed?
Do you feel that nothing is worth doing?
A decline in interest or pleasure in activities you once found fulfilling is a common sign of depression.
This loss of enjoyment can affect various aspects of your life, including work and personal relationships.
“G” is for Guilt:
Do you struggle with low self-esteem?
Are you overwhelmed by feelings of guilt or worthlessness?
Intense guilt and feelings of worthlessness can be debilitating and are significant indicators of depression.
These emotions can erode your self-worth and make daily tasks seem impossible.
“E” for Energy Levels:
Do you often feel fatigued or experience persistent burnout?
Chronic fatigue and a lack of energy, especially if it lasts for days, are common symptoms of depression.
This persistent exhaustion can hinder your ability to engage in daily activities.
“C” is for Concentration:
Do you frequently struggle with concentration or focus?
Difficulty concentrating or making decisions is a hallmark of depression.
This symptom can impact your productivity and ability to handle tasks effectively.
“A” for Appetite or Weight Fluctuations:
Have you noticed significant weight or appetite changes?
Are you eating much less or much more than usual?
Dramatic changes in appetite or weight—whether through loss of appetite or overeating—are common in depression and can affect your physical health.
“P” for Psychomotor Agitation or Retardation:
Have you become noticeably slower in your movements or thought processes?
Do you feel restless or unable to sit still?
Psychomotor changes can severely impact your ability to function at work or home.
This symptom involves either physical restlessness or significant slowing down.
“S” is for Suicidal Ideation:
Are you preoccupied with thoughts of death or self-harm?
Have you made plans to commit suicide?
Suicidal thoughts are a severe symptom of depression and require immediate attention.
If you are experiencing these thoughts, seek help from a mental health professional or go to the nearest emergency room right away.
Risk Factors for Suicide Include:
- Mental illnesses such as depression or bipolar disorder
- Social isolation, particularly in elderly patients
- Male gender
- Financial problems
- Impulsive or aggressive tendencies
- Job loss or legal issues
- Serious illness
- Substance abuse disorders
- Unsafe media portrayals of suicide
A Reminder About Professional Care
While SIGECAPS can offer valuable insights and support your journey, it’s crucial to remember that professional guidance is critical for managing depression effectively.
If you identify symptoms or patterns that concern you, seeking help from a healthcare provider is essential.
Combining self-assessment with professional care can lead to a more comprehensive and practical approach to mental health.
Using SIGECAPS to Manage Depression
Using SIGECAPS as a self-awareness tool can provide valuable insights into your mental health and help identify areas needing attention.
This approach can be a meaningful addition to your wellness toolkit.
In my own experience with depression, SIGECAPS was more than just a diagnostic tool—it became a lens through which I could better understand how to improve my physical and mental health.
Reflecting on these areas allowed me to develop effective personal growth and wellness strategies.
SIGECAPS – An Alternative Approach
While antidepressants can be life-saving, especially in severe cases, they are not the only option for managing depression.
If you’re experiencing mild to moderate depression or if medication hasn’t provided the relief you need, this article offers alternative strategies that may complement your current treatment—or, in some cases, serve as a standalone approach.
For those struggling with “treatment-resistant depression,” where medications haven’t been effective, or if you’re hesitant to start medication, exploring other avenues can be empowering.
It’s essential to be aware that while antidepressants can be beneficial, they may also have serious side effects, including suicidal thoughts.
These risks are noted on the warning labels of many antidepressants.
Discussing these side effects with a healthcare professional is crucial if you have concerns.
By using the SIGECAPS acronym, you might find, as I did, that this approach not only aids in managing your depression but could also help you reduce reliance on medications, especially if they haven’t been providing the relief you need.
So, if you’re looking for a way to manage your depression—whether as a complement to medication or as an alternative—exploring this roadmap could be a valuable step in your journey toward wellness.
When to Use the SIGECAPS Framework
The SIGECAPS checklist can be a powerful tool for lifting your mood—potentially even without medication—and sometimes can provide lasting relief.
If you’re taking antidepressants that haven’t been effective or if you’re experiencing adverse side effects, SIGECAPS can be a helpful tool alongside professional care and treatment options.
Many people face challenges with medications that don’t seem to work or come with unwanted side effects, such as:
- Insomnia, night sweats, or nightmares
- Loss of sensation in the lower extremities
- Hallucinations
- Suicidal thoughts
Speaking from personal experience, I understand how frustrating it can be when medication fails to deliver the promised relief or causes additional problems.
After years of struggling with these issues, I discovered that using SIGECAPS not only helped me identify the root causes of my depression but also guided me toward effective, natural solutions.
This roadmap isn’t just for those who have struggled with medication; it’s also valuable for anyone experiencing depressive symptoms without current treatment.
It can be a helpful tool in understanding and managing your mental health, whether as a standalone approach or in conjunction with other therapies.
Remember, if you’re currently on medication or experiencing significant depressive symptoms, consulting with a healthcare provider is crucial.
They can help you explore all available options and receive proper support.
The SIGECAPS Checklist – Practical Habits
In this section, you’ll find actionable steps based on the SIGECAPS framework to help manage your depression.
Integrating these strategies into your daily routine can provide valuable insights into your mental health and foster positive changes.
Understanding my application of the SIGECAPS checklist can be a game-changer for improving your mental health and well-being.
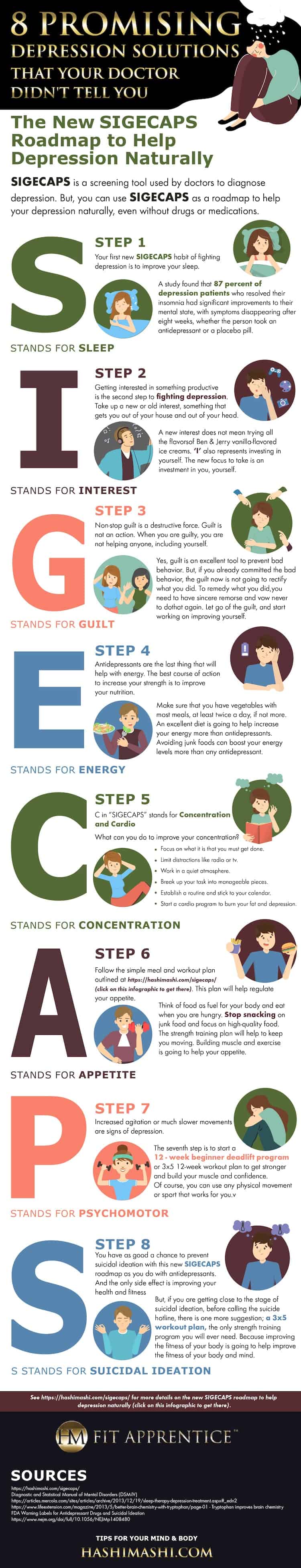
To help you visualize this process, we’ve put together a detailed infographic that breaks down each step of the SIGECAPS mnemonic.
This roadmap will walk you through the key aspects of managing your mental health, from sleep and interest to energy levels and strength training.
Take a moment to check out the infographic below, and then we’ll dive into some actionable tips you can start using right away.
How to Use SIGECAPS to Manage Depression
How to Apply the SIGECAPS Checklist
Step 1. “S” – Improve Your Sleep
Improving sleep quality is one of the most powerful strategies for boosting energy and managing depression.
Research has shown that sleep plays a crucial role in mental health, and enhancing sleep habits can significantly reduce depressive symptoms.³
In a study involving patients with depression, both those on antidepressants and those on a placebo, 87% of participants experienced significant improvements in their mental state by establishing better sleep habits.
Remarkably, their symptoms began to subside within just eight weeks.
The study’s lead author emphasized the importance of integrating sleep-focused therapy with standard depression treatment, stating: “The way this story is unfolding, I think we need to start augmenting standard depression treatment with therapy focused on insomnia.” 4, 5
How to Improve Your Sleep:
- Reserve Your Bed for Sleep: Avoid using your bed for activities that induce anxiety, such as work or watching the news. This practice helps establish a clear psychological connection between your bed and sleep.
- Establish a Sleep Schedule: Aim for a consistent bedtime around 9:30, 10, or 11 p.m., and keep your room dark and cool to enhance sleep quality.
- Practice Mindful Breathing Before Bed: Focus on your breathing, reflect on positive thoughts, and visualize positive experiences or things that bring you happiness, such as achieving your goals.
- Aim for 7-8 Hours of Sleep Per Night.⁶ Regular, quality sleep can help “reset” your mind and contribute to overall physical and mental well-being.
For more strategies on improving sleep quality, refer to Shawn Stevenson’s Sleep Smarter.⁷
The Walker Lab at the University of California, Berkeley, also emphasizes the role of sleep in cognitive and emotional health.⁸
Watch the following interview with Dr. Matt Walker for more in-depth insights into sleep science.
In it, he discusses the biology of sleep and offers personalized advice on improving sleep quality.
This video, part of the Huberman Lab Guest Series, provides valuable context and practical tips from a leading expert in the field.
Dr. Matt Walker: The Biology of Sleep & Your Unique Sleep Needs
Step 2. “I” – Find a New Interest
Discovering a new interest, particularly one that is engaging and productive, is a crucial step in combating depression.
If you are disinterested in many activities, don’t worry—reconnecting with your passions starts with just taking the first step.
Here’s how you can begin: Dive into something you think might interest you or revisit activities you once enjoyed.
It’s about getting out of your house and out of your headspace.
The goal is to revive your sense of curiosity and self-worth.
Remind yourself that you are exciting and worth investing in.
Finding new interests can be a powerful way to reignite your passion and combat depression.
Remember when you felt most engaged and try to reconnect with those feelings.
Investing in yourself is key!
Remember: Taking on a new interest doesn’t mean trying every Ben & Jerry’s ice cream flavor.
Instead, consider activities that enrich and add flavor to your life.
Here are some ideas:
- Strength Training: to improve physical fitness and improve mental well-being simultaneously, use resistance training exercises such as;
- Deadlifts
- Squats
- Bench presses
- Calisthenics exercises like pushups, pullups, bodyweight squats, and planks
- Pick Up a Musical Instrument: Learning to play an instrument can be both therapeutic and rewarding.
- Study a New Language: Expanding your linguistic skills opens up new worlds and cultures.
- Learn Photography: Capturing the world through a lens can be a creative and fulfilling pursuit.
Step 3. “G” – Let Go of Guilt
Persistent guilt can be destructive, hindering your ability to take positive action and eroding your inner peace.
Excessive guilt is like a prison; it confines you and prevents healing.
Understanding guilt involves recognizing whether it stems from a genuine violation of your moral code or something less clear.
If you’ve made a mistake, guilt alone cannot undo it.
The true remedy lies in sincere remorse, a commitment to change, and moving forward.
Here’s how you can manage guilt effectively:
- Acknowledge and Apologize: If you owe an apology or restitution, take action to make amends. If forgiveness isn’t granted, recognize that the matter is beyond your control.
- Seek Support: Share your feelings with a friend, family member, or mentor who can offer understanding and support.
- Forgive Yourself: Start by forgiving others, especially those close to you, including yourself. This process can help alleviate your feelings of guilt.
Powerful affirmations can assist in dissolving guilt:
- “I release the need to blame anyone, including myself.”
- “We are all doing our best with the understanding and awareness we have.”
- “Despite my struggles, I choose to love and accept myself.”
- “I am okay, and it’s safe to forgive myself.”
- “Today, I accept myself as I am and acknowledge the good I do.”
- “I am learning and growing each day.”
- “I am patient with myself.”
- “I love and approve of myself.”
- “I release self-blame and criticism. I don’t need these feelings anymore.”
- “I forgive myself for being too hard on myself.”
- “I deserve abundance and joy. I am good enough.”
These affirmations are based on Louise Hay’s teachings in her classic book, You Can Heal Your Life.
They can help you move past guilt and embrace self-acceptance.
Step 4. “E” – Eat Real Food for Energy
Diet Tips for Depression: Boost Your Energy
People taking antidepressants often experience lethargy, either as a side effect or a symptom of their condition.
Boosting your energy levels involves focusing on nutrition and incorporating exercise into your routine.
Prioritize Nutrition
Your diet is crucial—second only to sleep—in managing energy and overall well-being.
Opt for high-quality, nutrient-dense foods:
- Incorporate Vegetables: Aim to include vegetables in most of your meals, ideally at least twice a day—one meal with raw vegetables and another with cooked vegetables.
- Avoid Processed Foods: Processed and junk foods may offer temporary pleasure but often lead to increased fatigue and weight gain. Instead, choose whole foods that provide sustained energy.
Choose Complex Carbohydrates
Replace refined sugars and processed foods with complex carbohydrates, which are converted into lasting energy:
- Old-Fashioned Oatmeal
- Buckwheat (Kasha)
- Barley
- Quinoa
- Brown Rice
- Sweet Potatoes
- Potatoes
- Sprouted Grain Bread (e.g., Ezekiel Muffins)
These options help maintain stable energy levels and prevent the fatigue associated with sugary, processed foods.
Identify Food Sensitivities
Certain foods may affect your mood and energy levels. Common culprits include:
- Wheat
- Eggs
- Peanuts
- Dairy
For some individuals, these foods can exacerbate feelings of depression or listlessness.
Removing or reducing these from your diet may improve your overall well-being.
A Balanced Diet Over Medication?
While a nutritious diet alone may not be a substitute for antidepressants for everyone, it can significantly enhance one’s energy and mood.
Prioritizing healthy eating can help you feel more energized and positively impact your outlook on life.
Consider swapping out processed snacks for nutrient-dense options to fuel your body with energy.
A nutrition-focused approach supports your physical health and contributes to your mental well-being, giving you the strength to tackle each day with greater vigor.
Sample Meal Plan for Improved Energy
Breakfast: Start with a tall glass of water with a lemon wedge.
Have half a grapefruit and oatmeal with berries and nut butter.
Consider adding boiled eggs or a vegetable omelet.
Lunch: Enjoy brown rice, black beans, vegetables, and optionally turkey or chicken.
If needed, snack on fruit between meals.
Dinner: Choose sweet potatoes, salmon, and vegetables such as asparagus, spinach, or broccoli.
If you’re still hungry, have an apple.
Consistency: Establish regular meal times to help your body anticipate and utilize the fuel it needs throughout the day.
Research shows that a diet rich in whole foods, vegetables, and lean proteins can positively impact mood and energy levels, making it a crucial component in managing depression. 10
Step 5. “C” – Build Concentration with Mindfulness, Nutrition & Cardio
Tips to Enhance Your Focus
Concentration can be a struggle for those dealing with depression, often making daily tasks feel overwhelming.
Improving your concentration involves mental exercises, dietary adjustments, and incorporating physical activity into your routine.
Mental Exercises
- Mindfulness Meditation: Practicing mindfulness can help you stay in the present moment and improve your focus. Even just 5-10 minutes a day can make a difference.
- Puzzle Games: Engage in brain games like crosswords, Sudoku, or memory games to sharpen your cognitive skills.
More Tips to Improve Concentration
- Focus only on the next right thing to do.
- Limit distractions like radio or TV that cause you to zone out and avoid positive steps like exercise.
- Work in a quiet atmosphere.
- Break up your tasks into manageable pieces.
- Establish a routine and write it down—stick to your calendar.
- Start a Cardio Program: Engage in 20-30 minutes of cardio exercise daily.
Activities like running, cycling, or brisk walking can enhance concentration by boosting blood flow to the brain, improving mental clarity, and helping to manage depression. 20
Nutritional Support for Concentration
The foods you eat can directly impact your brain’s ability to concentrate. Focus on incorporating the following nutrients into your diet:
- Omega-3 Fatty Acids: In fish like salmon, walnuts, and flaxseeds, omega-3s are essential for brain health and can enhance cognitive function. Research published in Nature Reviews Neuroscience emphasizes the role of omega-3 fatty acids in maintaining brain health and improving cognitive function, particularly in mood disorders. 11
- Many people, including myself, have noticed a consistent improvement in mood after meals containing salmon.
- Antioxidants: Foods rich in antioxidants like berries, dark chocolate, and leafy greens help protect your brain from oxidative stress, improving focus and memory. Research indicates that a diet high in antioxidants is associated with better cognitive function and reduced symptoms of depression. 12
- B Vitamins: B vitamins, particularly B6, B12, and folate, play a crucial role in brain function. Sources include eggs, fish, poultry, and fortified cereals. Deficiencies in these vitamins have been linked to cognitive decline and increased risk of depression.13
Caffeine in Moderation
While caffeine can temporarily boost concentration, relying on it too much can lead to crashes and increased anxiety.
Opt for green tea over coffee for a gentler, sustained energy boost without the jitters. 14
Sample Meal Plan for Enhanced Concentration
Breakfast: Start your day with oatmeal topped with flaxseeds and blueberries. Pair it with scrambled eggs for an extra dose of B vitamins.
Lunch: Prepare a salad with leafy greens, walnuts, grilled salmon, and a citrus-based dressing. Add a piece of sprouted whole-grain bread on the side.
Dinner: Enjoy a quinoa and vegetable stir-fry with tofu or chicken and a small piece of dark chocolate for dessert (if you can control yourself!).
Step 6. “A” is for Appetite – Focus on Foods with Tryptophan
To help regulate your appetite and boost energy, follow the simple meal and workout plans outlined in this article.
Rethink your relationship with food by viewing it as “fuel for your body,” which encourages eating only when truly hungry.
Remember, your physical and mental health are interconnected, so don’t punish your body for your mind’s anxieties.
A poor diet can contribute to depression.
Therefore, reducing junk food and focusing on high-quality foods is essential.
Strength training will keep you moving, boost energy levels, and encourage healthier eating habits.
Building muscle through exercise can help regulate your appetite and improve your body’s craving for quality nutrition.
Proper Nutrition and Depression
Despite its importance, some psychiatrists might overlook the role of diet in mental health.
Good nutrition can be a key factor in overcoming depression, often as essential as medication.
Let’s look at how antidepressants function: Antidepressants commonly prescribed to increase serotonin levels in the brain include SSRIs (Selective Serotonin Reuptake Inhibitors) such as Prozac, Celexa, and Zoloft.
These medications block receptors that reabsorb serotonin, thus increasing its availability in brain cells.
Tricyclic antidepressants like Pamelor also help maintain higher levels of serotonin and norepinephrine, which can improve mood.
Increasing Serotonin Naturally
However, medication isn’t the only way to boost serotonin levels.
Diet plays a crucial role in creating natural improvements.
Consider whether your eating habits have reduced serotonin and contributed to depression.
Increasing serotonin naturally through diet, particularly with tryptophan-rich foods, can be highly beneficial.
Tryptophan is a natural amino acid essential for serotonin production.
Foods high in tryptophan can help normalize serotonin levels and improve mood, reducing depression and enhancing motivation. 15
Foods High in Tryptophan: 16
- Salmon and Tofu: Both can enhance mood. Ever notice a mood lift after good salmon? That’s why!
- Eggs: Can significantly boost blood plasma levels of tryptophan.
- Cheese: Varieties like cheddar and gruyere are excellent sources.
- Fish: Halibut, cod, flounder, tilapia, and tuna all contribute to better mood regulation.
- Nuts and Seeds: Walnuts, flaxseeds, and sunflower seeds are beneficial.
- Turkey and Chicken Breast: Known for their high tryptophan content.
- Dairy: Traditional milk, yogurt, and soy milk alternatives.
- Fruits and Vegetables: Include bananas, avocados, spinach, and peas.
- Whole Grains: Brown rice, red rice, barley, corn, and oats.
Incorporating these foods into your diet can provide the nutrients necessary to support your mental health naturally.
Step 7: “P” for Improve Psychomotor Skills with Exercise and Sports
Are you often feeling anxious, unable to sit still, or find your mind racing?
Do you also notice feelings of sluggishness or a lack of energy in your movements?
Engaging in Exercise: A Personal Journey
I’ve personally experienced the transformative effects of exercise while navigating my journey with depression.
effective method I found helpful was using this 12-week beginner deadlift program to build strength and confidence.
Regular strength training can help improve muscle tone, which supports your overall metabolism and energy levels.
It turns out that when you exercise, your body releases endorphins—these are natural chemicals that can boost your mood and promote a sense of well-being, akin to the effects of morphine. (WebMD)
As a result, you may feel better than ever.
It’s important to remember that the benefits of exercise can vary based on individual factors, such as the intensity of your workouts (Medical News Today).
Consider incorporating full-body compound movements like squats and deadlifts, which research has shown can help ease depressive symptoms.
For more details on how weightlifting helped my depression, see Best Exercise for Depression: How Deadlifts Saved My Life.
However, remember that there are many ways to be active!
Any form of movement—walking, calisthenics, swimming, CrossFit, or practicing yoga—can be beneficial, so find what works best for you.
The author Rich “Hashi Mashi” Deadlifting at 64
Step 8: “S” is for Strength Train instead of Suicidal Ideation
Instead of focusing on thoughts that harm your body, channel your energy into building it up!
Suicidal ideation is a serious and complex topic, often exacerbated by the very medications prescribed to manage depression.
Many antidepressants carry an FDA-required warning about the potential for suicidal thoughts as a side effect.
FDA warning label for antidepressant Lexapro – Image Credit: Time Magazine 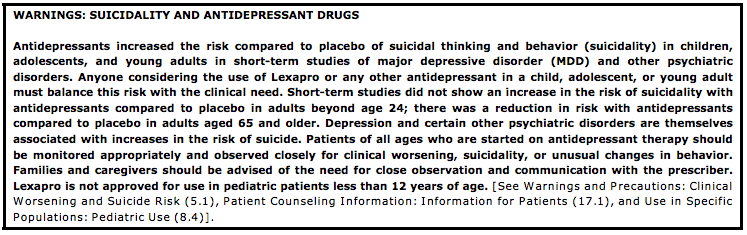
However, you may be able to avoid these thoughts—or prevent acting on them—by following the SIGECAPS checklist.
This approach can complement other depression treatments and improve mental well-being.
The only “side effects” of this program are improved health, fitness, energy, and focus.
Strength training was a critical factor in helping me to stop suicidal ideation, regain mental clarity, and eliminate my need for antidepressants.
Beyond my personal experience, the science backs this up.
A meta-analysis of 33 clinical trials involving 1,877 participants found that resistance exercise training significantly reduces depressive symptoms.
According to the researchers, “The available empirical evidence supports resistance exercise training as an alternative and/or adjuvant therapy for depressive symptoms.” 17
Can Lifting Weights Help Combat Depression and Anxiety?
Watch: What Science Says About Strength Training and Depression.
Strength training has been a game-changer for many people facing depression and anxiety — myself included as mentioned above.
In this video below, Dr. Layne Norton discusses a meta-analysis published in JAMA Psychiatry, which reviewed 33 clinical trials and found that resistance training significantly reduces depressive symptoms—even in individuals without a clinical diagnosis.
This scientific review highlights how strength training can be a powerful tool for improving mental health and managing depression naturally.
In this video, you’ll see how using physical discipline like weightlifting can clear the mind, rebuild confidence, and support emotional resilience.
If you’re searching for ways to lift both your body and your spirits, this inspiring look at strength training’s impact on mental health might be the spark you need:
SIGECAPS to Manage Depression and Anxiety – Wrapping Up
Incorporating the SIGECAPS checklist into your daily routine offers a powerful way to combat depression and build a stronger, healthier life.
While this roadmap is valuable for anyone facing mental health challenges, it holds particular relevance for men over 50.
This group often faces unique risks for depression due to factors like retirement, health issues, and social isolation.
Studies have shown that depression affects up to 10-15% of men in this age group. 18,19
Combining regular physical activity, resistance training, and mindful nutrition can significantly improve your mental and physical well-being.
To regain your health, start small with daily walks and gradually progress to structured strength training routines like calisthenics, dumbbell workouts, or deadlifting.
Remember, this journey is about more than lifting weights—it’s about lifting your spirits and finding the resilience to overcome life’s challenges.
Whether you’re beginning this journey or looking to enhance your fitness regimen, these strategies can serve as your foundation for lasting change.
Always consult with your healthcare provider before making significant changes to your routine.
You’ve taken the first step by exploring this roadmap.
Now, it’s time to put these principles into practice and witness their transformative power in your life.
What’s Next: Exploring More Paths to Strength and Wellness
While deadlifting played a crucial role in helping me overcome obesity and depression, it’s important to remember that it’s not the only path to health and well-being.
Strength training can take many forms, and your best approach might differ from what worked for me.
Here are some excellent resources to help you get started with strength training, whether you’re using a barbell, resistance bands, or your body weight:
- How to Weight Lift for Weight Loss: A Plan That Works: Discover how lifting weights can be an effective tool for losing weight and improving mental health.
- Strength Training for Men Over 50 + Full Body Workout: Tailored exercises to maintain strength and vitality as you age, focusing on physical and mental resilience.
- 5×5 Workout for Over 50: The Pros + Cons You Need to Know: A structured program that combines simplicity with effectiveness, perfect for building a solid foundation.
- 7 Best Compound Exercises for Muscle and Strength + Workout: Learn about the most effective compound exercises that target multiple muscle groups, maximizing your workout efficiency.
- Calisthenics Workout for Beginners at Home: No equipment? No problem. This guide helps you use your body weight to build strength and flexibility at home.
- 8 Great Dumbbell-Only CrossFit Workouts at Home: A versatile workout that requires just a pair of dumbbells, perfect for a quick and practical training session.
- 7 Spectacular Ways Swimming Transforms Your Body: Swimming can be a powerful full-body workout that boosts physical and mental health.
Each resource offers a unique approach to incorporating strength training into your routine, allowing you to choose the one that best suits your lifestyle and goals.
Begin with daily walks and take rest days from resistance training on Tuesday, Thursday, and the weekend to allow your body to recover and rebuild.
Walking is a simple, accessible way to enhance physical and mental well-being.
If you’re interested in diving deeper into deadlifting and its benefits, here are some additional resources that might interest you:
- WHY Deadlifts are So Good For You: The 7 Mighty Muscle Groups Deadlifts Work
- 37 Remarkable Benefits of Deadlifts to Unleash Your Fitness Fast
- 27 Sensational Ways How Deadlifts Change Your Body and Mind
- How to Deadlift for Beginners – A Step-by-Step Guide
- The Simplest DIY Deadlift Platform for Beginners
Improving your body’s fitness will enhance your mind’s fitness as well.
Begin your journey today, and don’t hesitate to share your stories and questions.
As you embark on this path, it’s crucial to consult with your primary care physician about using the SIGECAPS checklist, which integrates strength training, nutrition, and mindfulness to support your overall health and wellness.
If this adaptation of SIGECAPS has helped you manage your fitness and depression, I’d love to hear about your experiences.
Feel free to reach out and share how integrating these practical tips has impacted your life.
Your story could help someone else cross the bridge from depression to a new life.
While self-care strategies like SIGECAPS can support mental wellness, they are not a replacement for professional mental health care.
If you’re experiencing severe depression or thoughts of self-harm, seek immediate help from a licensed mental health provider.
A Note of Caution: If you or someone you know is struggling with severe mental health issues or suicidal thoughts, please seek professional help immediately. There are resources available to support you, including the National Suicide Prevention Lifeline at 1-800-273-TALK (1-800-273-8255).
Footnotes
³ The Role of Sleep in Depression – Science Direct
4 Improving Sleep Quality Leads to Better Mental Health – National Library of Medicine
5 Sleep Therapy Seen as an Aid for Depression – New York Times
6 National Sleep Foundation’s sleep time duration recommendations: methodology and results summary
8 The Role of Sleep in Cognition and Emotion – Walker Lab – University of California, Berkeley
9 Food and mood: how do diet and nutrition affect mental well-being? – National Library of Medicine
10 Diet and Depression – Harvard Health Publishing
12 The Nutrition Source – Antioxidants – Harvard School of Public Health
13 B Vitamins and the Brain: Mechanisms, Dose, and Efficacy—A Review – Nutrients Journal
14 Effects of caffeine on human health – Food Additives and Contaminants Journal
15 How Tryptophan Boosts Your Sleep Quality and Mood – Healthline
16 Foods high in tryptophan – Med-Health.net
17 Association of Efficacy of Resistance Exercise Training With Depressive Symptoms – JAMA Psychiatry
19 Percentage of U.S. men with a major depressive episode in the past year as of 2022 by age – Statista
20 Be smart, exercise your heart: exercise effects on brain and cognition – Nature Reviews Neuroscience